TORONTO — The signs were there, but Lidia Vetturetti says her mother refused to consider the possibility she had Alzheimer's.
By the time she was diagnosed five years ago, the disease was so advanced Nicole Vetturetti was forced to enter a full-time care facility the following year.
Lidia Vetturetti believes her mother's rapid decline was accelerated by the belief there was no point seeking help earlier.
But now, she says there's real hope for other patients and their families, thanks to a landmark $16.7-million grant announced Monday that will speed up development of targeted treatments of a variety of brain disorders — including Alzheimer’s, brain cancer and ALS.
Just the prospect that new research could revolutionize the way doctors tackle hard-to-treat conditions is powerful stuff, she says, and would have been enough to make a difference in her own family's life.
"It would have changed everything. I would have pushed her to go (to the doctor) even sooner because I would have said, 'There's trials. As soon as we can, let's try it. It might stop this. It might slow down.' And we might have had longer with her," says Vetturetti.
"She's still here, but she's not really. I lost her a long time ago."
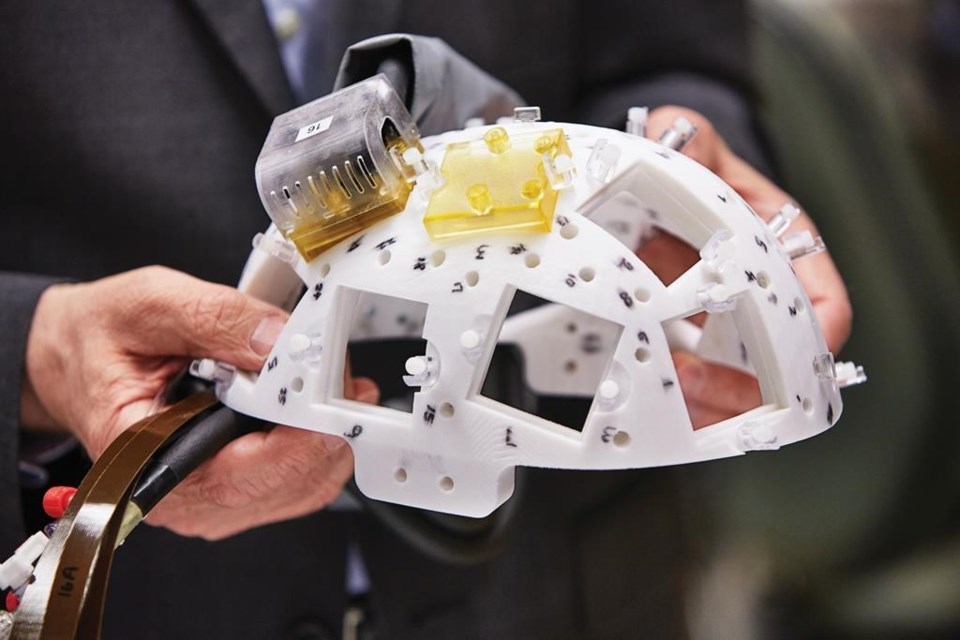
Sunnybrook Hospital says the funds from the W. Garfield Weston Foundation will help create a new type of focused ultrasound device that can more efficiently bypass the blood-brain barrier in delivering treatments.
The Toronto hospital will test the helmet-like device on three brain disorders, including Alzheimer's disease, breast cancer that has spread to the brain, and glioblastoma — the deadliest and most common brain tumour.
The blood-brain barrier is a tightly packed network of vessels meant to protect the brain from toxins. But it can also be a major obstacle in many conditions because it prevents potentially helpful agents from entering the brain — such as chemotherapy, antibodies, stem cells or gene therapy.
The hospital already does focused ultrasound treatments but neurosurgeon Dr. Nir Lipsman says this new device could allow doctors to deliver medication directly to a brain tumour, and allow more targeted treatment in multiple areas, with less medication and fewer side effects.
For one thing, the helmet-like prototype would be specifically fitted to each patient and wouldn't need an MRI for guidance, which is the current practice.
The new device also wouldn't require a patient to wear a painful frame to immobilize the head as is common now, in which four pins are inserted under local anaesthetic for several hours.
"Many of the treatments that we're envisioning are serial treatments, which means the treatments will happen over time repeatedly. And the more comfortable you can make the procedure, the more streamlined and efficient you can make it, the shorter in duration you can make it, the better it will be for patients," said Lipsman.
The hospital's foundation is trying to raise the rest of its $33-million goal for the Weston Family Focused Ultrasound Initiative.
Research like this can offer powerful hope to patients and families grappling with a frightening diagnosis, adds Vetturetti.
"Hopefully in the future people won't have to go through what I've gone through with my mother or that she has gone through as a result of this illness," she says.
"It gives me hope as well that if, God forbid, I ever was to get this diagnosis, that maybe there would be hope for me, or my children."
This report by The Canadian Press was first published on March 2, 2020
Cassandra Szklarski, The Canadian Press