WARNING: This article contains details that may disturb some readers. If you or someone you know needs to speak with someone, please call Kids Help Phone at 1-800-668-6868 or 9-8-8 for the Suicide Crisis Helpline.
By every measure, Brett Provenzano should be a 29-year-old man today. He had dreams of becoming a police officer or a teacher, but his life was cut short in 2010 at the age of 15 when he died by suicide.
It has been 14 years since Brett's untimely death. He has been gone from this earth for almost as many years as he lived. His mother, Gail Provenzano, mourns him every day and has taken concrete steps to bring meaning to his death.
"He was just a typical boy going through life changes at 15 in high school," Provenzano said. "Brett was the kid who, when we go through the mall at Christmas time would give money to the Salvation Army or if a bird flew into my parents' house he would take care of it."
In Grade 9, Brett was six-foot-one and played hockey, but Provenzano said his true love was football. He played Sault Minor Football as well as for the St. Mary's College junior team.
Losing Brett in such a tragic manner hit Provenzano and her family in several ways.
"I missed seeing him get married and having kids. I missed watching him possibly go off to college or university to play football. I just missed what every other parent gets," said Provenzano.
It also meant that part of her life — being a football mom on the sidelines — was also gone.
"We had a big circle of friends and when Brett died we lost a great deal of friends, too," she said. "It's not that they never contacted me, it's just when you lose a child you're taken away from that life. Now there's no more hockey. There's no more football. There's no more high school. There's no graduation. There's no more of anything where those connections are."
Brett is just one of many teenagers in the province who died by suicide between 2010 and 2022, with northern Ontario's rate of death by intentional self harm four times higher than the Ontario average, according to data from Ontario's Registrar General provided to Village Media journalist Patrick Cain.
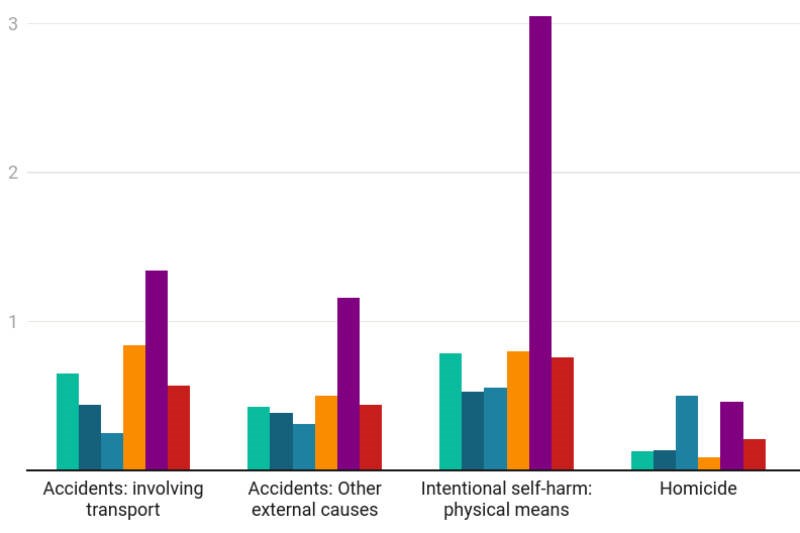
The following graph shows death rates per 1,000 among people aged 13 to 19 between the years 2010 and 2022. Among the graphs showing select causes of death, northern Ontario stands out with a rate of death by intentional self harm - physical means that is four times higher than the province as a whole.
Local leaders say those statistics are just another example of the health inequities between communities in northern versus southern Ontario.
Those statistics don't come as a surprise to Ali Juma, executive director of Algoma Family Services (AFS). His agency takes a leading role in addressing the mental health issues faced by youth in the region. His organization relies on stats from Algoma Public Health (APH) that also show the problems of mental health and intentional self-harm are worse here than in southern Ontario.
APH's recently released Community Health Profile notes that hospitalization rates due to self-harm have been notably higher in Algoma compared to Ontario for the last several years.
"The disparity here is really a matter of health equity," said Juma. "Young people in our community, compared to southern Ontario, do not have the same access to much-needed resources and services and there's a consequence to it."

Chief among Juma's concerns is a total lack of full-time child psychiatrists practicing in Algoma District. Most youth who require psychiatry in the Sault and surrounding area are serviced by Telehealth Ontario by telephone or, in some cases, by a psychiatrist who usually specializes in treating adults.
APH's Community Health Profile notes that in 2019, the longest wait for counselling and therapy for a person under 18 years of age in Algoma was 370 days — more than a full year. The wait time for intensive treatment was 632 days — more than a 20-month wait.
In contrast, the average wait time for youth in southern Ontario for counselling and intensive treatment was 67 days and 92 days, respectively.
"If you think of children in southern Ontario that have access to child psychiatry, it's a very different scene," said Juma, who notes AFS has seen children as young as eight years old who have attempted some form of self-harm.
The problem is compounded by the current shortage of primary care available to Sault residents, especially after the Group Health Centre announced earlier this year that thousands of patients would lose their current doctor or primary care provider.
"In Sault Ste. Marie right now we have over 10,000 patients that have been de-rostered," said Juma. "Until we actually attend to that, the tragedy is, I don't see a change in those numbers — if anything we will potentially see an increase."
AFS typically becomes involved if a youth presents to Sault Area Hospital (SAH) with suicidal ideation or after a suicide attempt. It can also begin a file if it is made aware of a concern about a youth from one of the four school boards that service the area, but that process is only enacted with consent.
About 10 years ago, Darryl Fillmore was the manager of intensive treatment services at AFS, where he worked on an initiative allowing the four local school boards to more easily share valuable information about at-risk youth between themselves, Algoma Family Services and Sault Area Hospital. Currently, he is the mental health lead for the Algoma District School Board.
In some cases, said Fillmore, students would receive treatment for suicidal ideation or an attempt at self-harm and then return to the school environment, with school staff unaware there was a problem and without a way to support that vulnerable student.
"Historically in our region — and it continues to be the truth throughout the province — it is happening without much information exchange at all, and that is very concerning," said Fillmore.

The initiative to streamline information sharing between agencies hit a snag that necessitates consent be given by a student or their family before the board can share mental health information about that student — that snag was privacy legislation.
"We do have the ability to communicate when there is imminent risk that supersedes confidentiality all the time," noted Fillmore.
Despite the need for consent to share with other agencies, Fillmore said the system that was built does a good job integrating the information with partner agencies and is a service many regions do not have access to.
"I talked to other [mental health] leads when we're in provincial meetings, and they are constantly astounded that we have been able to engage in this wonderful partnership here in Algoma," said FIllmore. "We really believe that it's something to be very proud of as a community and ultimately very helpful to the families and students involved."
In 2023, Dr. John Heintzman was announced as the new chief of staff for SAH. After a career as a child and adolescent psychiatrist, Heintzman came out of retirement and moved back to Sault Ste. Marie just over a year ago after spending 19 years as chief of psychiatry and medical director of the Mental Health and Addictions Program at Grand River Hospital in Kitchener/Waterloo.
Recognizing the shortage of psychiatry available in the Sault, Heintzman began balancing his responsibilities as chief of staff with spending one day per week acting as a child and youth psychiatrist at the hospital.
"It was a real struggle to move back to the Sault and and not spend more time doing clinical work, but at the same time the chief of staff position was a very interesting challenge," said Heintzman. "I'm trying to find a balance between the two."
Sault Area Hospital's Child and Adolescent Psychiatry (CAP) unit serves patients under the age of 18 who are experiencing acute symptoms of serious mental illness that can't be managed in the community.
Not all hospitals have a CAP unit and Heintzman said the unit at SAH factored into his decision to take on the role of chief of staff.
"I was very grateful when I started exploring the opportunity to know that investment had occurred and that there was a CAP unit here," he said.
Heintzman said all youth have value and problems can be improved — if they reach out to ask for help.
"I think oftentimes youth kind of feel like they're caught and there's no solution and kind of trapped in a box — partly because their brains aren't fully developed," he said.
"They don't think in a problem-solving type of way and latch on to one thing and they go with it. I'd just like to get that message out, that even if you don't see a solution other people might and talking about it can help."
In recent years, Provenzano has taken her grief and tried to mould it into positive change and to support others.
She participates in support groups to help others who are going through similar tragedies to her own and by participating in the Community Strong Race Weekend, which raises money for the Algoma Family Services Foundation to bring awareness to physical and mental health challenges in the community.
Although Provenzano is nearing retirement, she has been focusing her energy on earning a graduate certificate in addictions and mental health through Algonquin College with the hopes of assisting others who are experiencing similar challenges as what her family went through.
"When I retire either next year or the year after I can maybe help somebody before they take that one last step," she said.