EDITOR’S NOTE: A version of this article originally appeared on The Trillium, a Village Media website devoted to covering provincial politics at Queen’s Park.
One in every 10 patients admitted to a hospital in Ontario from an emergency department waits at least two days before they get a bed, according to an internal government document.
The nearly 50 hours from the moment those patients walk in the door to the time they're in an inpatient bed is a historical high. The long waits on stretches in emergency departments result in actual harm to the province's most vulnerable, emergency physicians told The Trillium.
"They're sick, they're frail, they've come in late," said Alan Drummond, an emergency physician in Perth, who had four patients on stretchers in his small, rural emergency department the day he spoke with The Trillium. "They need to be admitted. They're stuck in a hospital hallway for 24, 36, 48 hours, and waiting for that hospital bed to materialize.
"And while they're there, they suffer increasing complications in terms of their medical illness. They have delayed access to the treatments that would be necessary should they have been admitted. They develop delirium. They get totally confused. Their dementia gets worse. And we know there's a mortality rate — people actually die as a result of that prolonged wait for bed admission."
Raghu Venugopal, an emergency physician in Toronto, described what he saw before speaking with The Trillium on Tuesday when the emergency department was too busy for paramedics to offload their patients: rows and rows of stretchers "filled with silver and gray-haired senior citizens silhouetted on Orange EMS blankets."
"I will physically go see that patient, I will see them in the corridor, I will see them on the paramedic's stretcher, I will see them in the back of a triage office or in the waiting room," he said. "But no investigations or treatments can commence unless it's a special case — in other words, unless they are very, very sick."
Ontario Health tracks emergency department metrics monthly and charts them. While the figures are commonly shared in health-care administration in a "provincial summary" report, the document is labelled "not to be distributed without express permission from OH."
The Trillium obtained a copy of the latest report and spoke with three emergency physicians about what it means.
"This report paints a picture of some of the worst emergency department performance in our province's history," said Adil Shamji, a Toronto emergency physician and a Liberal MPP, echoing the others.
"This is not a unique phenomenon," said Venugopal, citing concerns about overcrowded emergency departments dating back to the days of Premier Bob Rae. "This is Ontario history. However, what stands out clearly from the data and from what physicians across Ontario are seeing is this is the worst experience compared to any provincial administration's leadership in the history of Ontario."
The charts below come from the provincial summary report by Ontario Health.
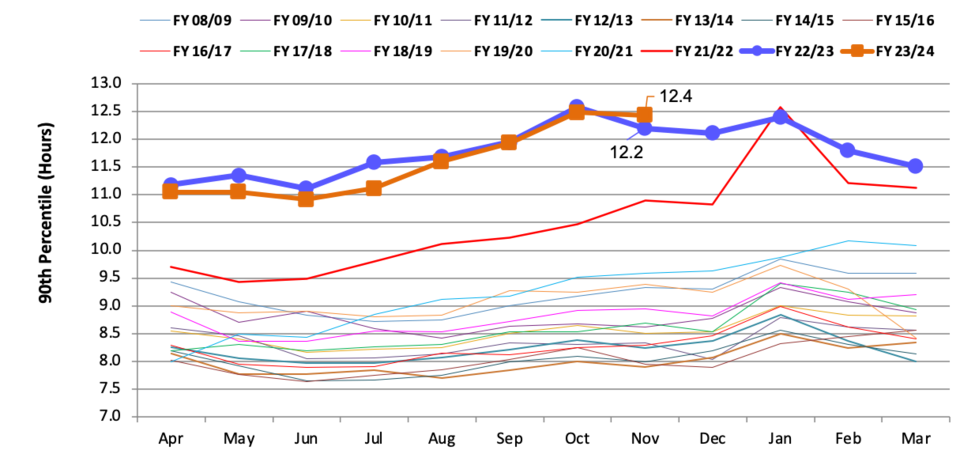
Provincial 90th Percentile Emergency department Length of Stay / Ontario Health
This chart shows the length of stay in Ontario emergency departments over time for the 90th percentile patient — that is, if you lined up 100 patients from shortest to longest time in the emergency department, this is the time the 90th person spent there — 10 per cent spent longer, the rest lower.
The orange line is this year. The blue is last year. The thinner lines are previous years, dating back to 2008.
This year and last year are significantly higher than any previous year on record.
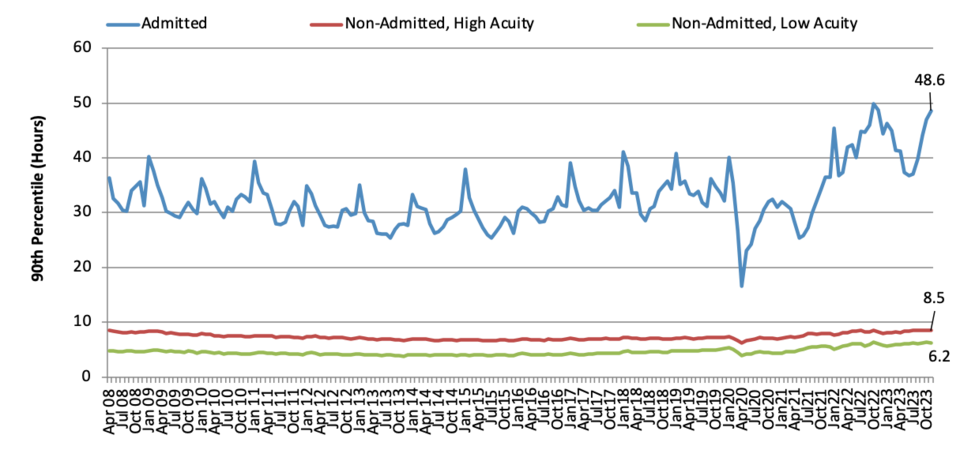
Provincial 90th Percentile Emergency Department length of Stay Trend by Patient Type / Ontario Health
This chart also shows the length of stay in Ontario emergency departments over time for the 90th percentile patient — but it breaks it down by patient type. The blue line represents those who are admitted to the hospital, the red line is high-acuity patients who are not admitted and the green line is low-acuity patients. All of the doctors who spoke with The Trillium identified the time it takes to admit patients as the core problem and said it's due to a lack of available beds.
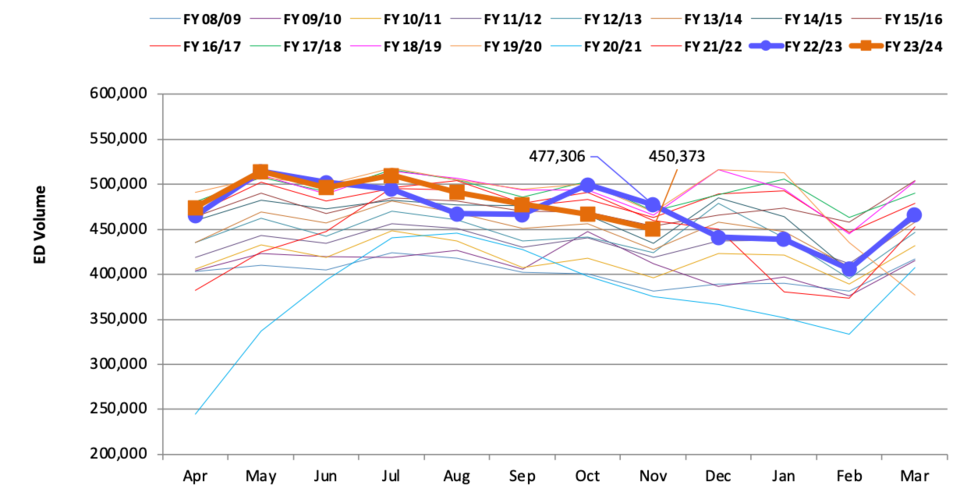
Provincial Emergency Department Volumes / Ontario Health
This chart shows the longer waits aren't due to more patients entering emergency departments, with the thick lines denoting this year and last roughly in line with years past, even as the population increases. Both Venugopal and Drummond said it puts the lie to the idea that the perception that low-acuity patients flooding emergency departments when they should be seeing a family doctor or walk-in clinic are the problem. Instead, it indicates patients' needs are more acute now than in the past. Shamji called the fact that wait times are rising apart from patient volumes the "most damning thing" about the report.
Response from the Minister of Health
“Ontario is leading the country with some of the shortest wait times in Canada, and last year, we had a record-breaking year, adding over 17,000 new nurses, nearly half of whom are internationally educated, and 2,400 physicians to our healthcare workforce. But we know more needs to be done, that’s why with our Your Health plan, our government is connecting more Ontarians to the care they need, when they need it," said spokesperson Hannah Jensen, on behalf of Health Minister Sylvia Jones.
"We have increased our investment by $44 million this year (23/24) to reduce emergency department wait times through local, innovative solutions, launched the Models of Care Innovation Fund to support innovative staffing models, allowing hospitals to use their staff to their full potential, while breaking barriers to make it easier for internationally and interprovincially educated healthcare workers to register and practice in Ontario, removing financial barriers for nurses looking to upskill, creating mentorship opportunities through the Clinical Scholar Program.
"Through our minor ailment initiative along with expanding 9-1-1 models of care we are also ensuring patients can connect to the care they need while avoiding unnecessary trips to the emergency room.”
This is part one of a series. The next will dive into the causes and solutions to the problem.
